The use of computerized healthcare data has revolutionized storage, access, and application of medical information. Digital Health Records (DHRs) or Electronic Health Records (EHRs) refer to organized sets of patient information in a digital environment that can be transmitted across healthcare institutions. They hold the potential to enhance efficiency, precision, and coordination of patient care. But their implementation has also created concerns about cost, privacy, and ease of use. This paper assesses whether or not digital health records are an asset or liability to healthcare systems.
Benefits of Digital Health Records
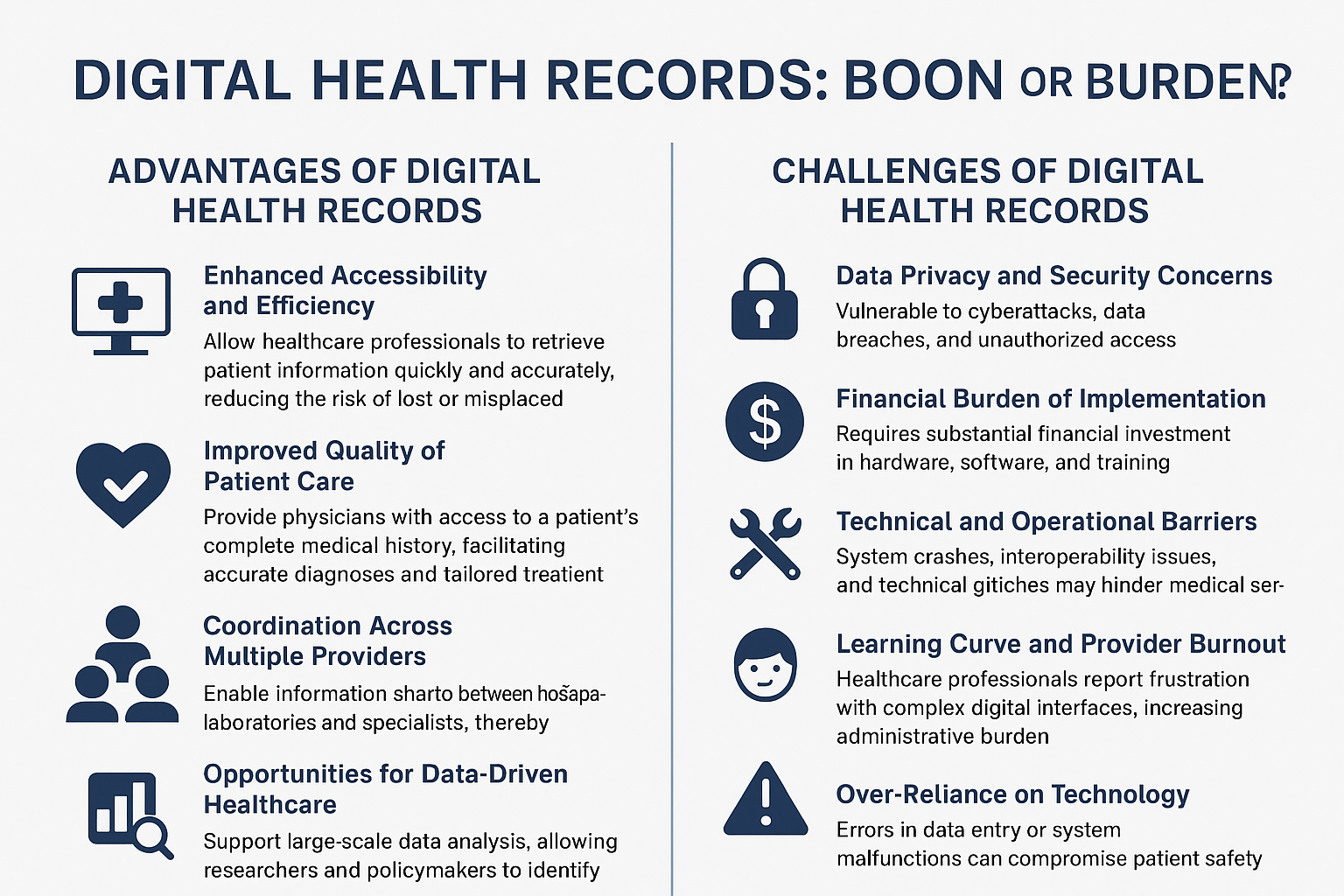
1. Improved Accessibility and Efficiency
DHRs enable healthcare workers to access patient data in a timely and precise manner, minimizing the chances of lost or mislaid documents. EHRs have been proven to enhance workflow effectiveness and time management in medical practice (Menachemi & Collum, 2011).
2. Enhanced Quality of Patient Care
Immersive digital records grant clinicians the ability to access a patient’s full medical history, support precise diagnoses, and develop personalized treatment protocols. There is evidence that EHR implementation is linked with improved management of chronic diseases and fewer medication errors (Buntin, Burke, Hoaglin, & Blumenthal, 2011).
3. Coordination Across Multiple Providers
Patients receive care from a number of healthcare providers. Digital records facilitate sharing of information among hospitals, laboratories, and specialists, thus enhancing continuity of care (Campanella et al., 2016).
4. Opportunities for Data-Driven Healthcare
DHRs facilitate big data analysis, enabling researchers and policymakers to detect disease trends, forecast outbreaks, and plan public health interventions (Kruse et al., 2016).
5. Environmental and Logistical Benefits
Conversion of paper-based to computerized systems minimizes physical storage needs, reduces administrative expenses, and encourages environmentally friendly practices.
Digital Health Records Challenges
1. Data Privacy and Security Issues
Computerized records are susceptible to cyber intrusions, data breaches, and unauthorized data access. Meeting data protection standards like HIPAA (Health Insurance Portability and Accountability Act) continues to pose a great challenge (Wager, Lee, & Glaser, 2017).
2. Implementation Cost Burden
Implementation of EHR systems calls for significant investment in hardware, software, and training. Rural healthcare facilities and small clinics usually struggle to maintain the costs (Adler-Milstein & Huckman, 2013).
3. Technical and Operational Barriers
Crashing of systems, interoperability, and technical faults could impede medical care. Additionally, failure to implement standardized platforms can result in patient data fragmentation (Campanella et al., 2016).
4. Learning Curve and Provider Burnout
Health care providers frequently comment on frustration caused by complicated digital interfaces, which can add administrative workload and diminish the time spent on direct patient care (Shanafelt et al., 2016).
5. Over-Reliance on Technology
System failures or data entry errors can undermine patient safety. Excessive reliance on digital systems without proper checks can blunt clinical judgment.
Discussion
The potential advantages of digital health records—everything from enhanced access and coordination to information-driven insights—are great. Yet their restrictions, especially regarding privacy, expense, and usability, must not be overlooked. Policymakers and health care facilities need to invest in secure, interoperable, and easy-to-use systems, while also providing proper training for healthcare professionals. Resolving these matters is essential for optimizing the value of digital records while reducing their drawback.
Conclusion
Digital Health Records are both opportunity and threat. They could be a blessing in terms of patient safety, efficiency, and public health promise, but they could be a curse if problems involving cost, privacy, and provider usability are not managed. The balance is finally a function of thoughtful implementation, continuous assessment, and compliance with ethical and regulatory guidelines.